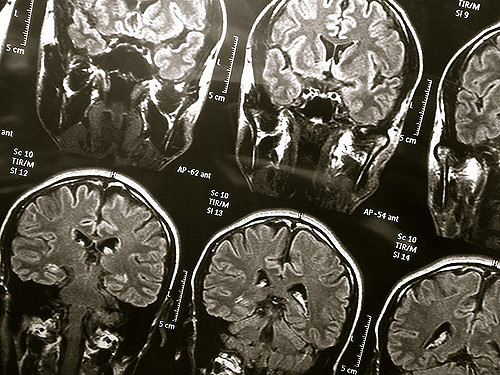
Alzheimer’s disease could be caused by the brain’s natural defenses against bacteria and infections, a new study suggests. Alzheimer’s disease is the most common type of dementia, with an estimated 46.8 million people worldwide living with dementia in 2015. The new study, which is the first to investigate the anti-microbial action of human beta-amyloid in living animals, revealed some promising results.
For the past 30 years, many scientists believed that plaque, the mysterious hard little balls that appear on the brains of people with Alzheimer’s, is simply the brain’s way of collecting and disposing of its trash. However, according to scientist at Harvard University, it is possible that the plaque is part of the brains defense against infection.
Dr Robert Moir, from Massachusetts General Hospital, said that “Neurodegeneration in Alzheimer’s disease has been thought to be caused by the abnormal behaviour of A-beta molecules, which are known to gather into tough fibril-like structures called amyloid plaques within patients’ brains,” stating also “this widely held view has guided therapeutic strategies and drug development for more than 30 years, but our findings suggest that this view is incomplete.”
According to the study, when the brain encounters an infection, including ones that are too mild to elicit symptoms, the brain’s defense system rushes to stop the infection by making and trapping it in a sticky cage made of proteins, called beta amyloid. When the virus dies, the cage of proteins remains in the brain and is seen as plaque – the hallmark of Alzheimer’s.
Although it is still early days, Alzheimer’s experts not associated with the study are excited at the prospects of this latest theory. “It is obviously outside the box,” said Dr. David Holtzman, a professor and the chairman of neurology at the Washington University School of Medicine in St. Louis. “It really is an innovative and novel study.”
The Harvard group’s data from the study, which was published Wednesday in the journal Science Translational Medicine, strongly supports the scientists’ hypothesis and could potentially lead to methods of preventing and treating this degenerative brain disease.
To test their theory, the scientists decided to observe the sequence in neurons growing in petri dishes as well as in yeast, roundworms, fruit flies and mice. Plans and funding to determine whether a similar sequence occurs in humans have already be set into motion.
Traditionally, scientists believed that the proteins were simply garbage that accumulates in the brain with age; however, Robert D. Moir, of Harvard Medical School and Massachusetts General Hospital, had an idea about the function of amyloid proteins when he noticed that they looked a lot like proteins of the innate immune system – the body’s first line of defense against infections.
The proteins of the innate immune system trap microbes — viruses, fungi, yeast and bacteria – allowing white blood cells to easily tackle the infection. In collaboration with Rudolph E. Tanzi, also at Harvard Medical School and Massachusetts General Hospital, Moir began to test whether “amyloid trapped microbes in living animals and if mice without amyloid proteins were quickly ravaged by infections that amyloid could have stopped,” the New York Times reports.
The study, which was funded by the National Institutes of Health and the Cure Alzheimer’s Fund, found that the amyloid proteins within the mice trapped the microbes. Meanwhile, the mice that did not make beta amyloid succumbed more quickly to the infection, and did not make plaques.
“Overnight, the bacteria seeded plaques,” Dr Tanzi said. “The hippocampus was full of plaques, and each plaque had a single bacterium at its center.”
However, as you can probably guess, not everyone that has a brain infection develops Alzheimer’s. According to the new theory, the reason lies with the brain’s ability to clear out the balls of beta amyloid after they have killed microbes, Dr Tanzi said.
The Cure Alzheimer’s Fund is starting a large collaborative project that will use gene sequencing technology to carefully search for microbes in people who had Alzheimer’s and those who did not. In addition, the researchers will also look for microbes in plaques found in human brains.
Dr Moir said “Our findings raise the intriguing possibility that Alzheimer’s pathology may arise when the brain perceives itself to be under attack from invading pathogens, although further study will be required to determine whether or not a bona fide infection is involved.
“It does appear likely that the inflammatory pathways of the innate immune system could be potential treatment targets. If validated, our data also warrant the need for caution with therapies aimed at totally removing beta-amyloid plaques.
“Amyloid-based therapies aimed at dialling down but not wiping out beta-amyloid in the brain might be a better strategy.”
Image: Flickr, wyinoue
You want to support Anonymous Independent & Investigative News? Please, follow us on Twitter: Follow @AnonymousNewsHQ
This article (Promising Study: Scientists May Have Just Found The Cause Of Alzheimer’s Disease ) is a free and open source. You have permission to republish this article under a Creative Commons license with attribution to the author and AnonHQ.com.




